Your Ibuprofen is Killing You
We’ve all seen the commercials. A middle aged man is playing [inset youthful sport here] and at then you see him gripping his [knee, wrist, shoulder, back] in pain and discomfort. There’s a voiceover of how much it sucks getting old. Then – a promised solution – 2 of this or that tablet, a few times a day. The commercial ends with the middle-aged man playing that same sport with grace and skill, laughing with his friends, and just loving life. The message in these commercials are clear. Got pain? Take an ibuprofen. Got pain every day? Buy in bulk.
Now, I’m not one of those anti-drugs and anti-surgery chiropractors by any means, but I have a strong hunch that those daily aches and pains aren’t caused by an ibuprofen deficiency. Nevermind that these pills aren’t actually fixing or reversing whatever’s causing the pain. What’s more concerning to me are the hidden dangers of these pills.
Ibuprofen, Aspirin, and Naproxen kill about 16,500 people a year.
Here are some fun facts…
- Every year, 100,000 people end up in the hospital because of NSAIDs and about 16,500 of them die from an NSAID toxicity.
- In 2007, 80,000 phone calls a day were made to poison control centers because of NSAIDs.
- Chronic NSAID use is the 15th leading cause of death in the USA.
NSAIDs are dangerous because chronic use can cause…
- Slow-bleeding stomach ulcers
- Liver and kidney disease
- Autoimmune diseases
- Degenerative Joint Disease (ironic when you consider most people take them for arthritis)
- Decreased immune response to bacteria and viruses
Symptoms of NSAID toxicity include…
- Stomach Ulcers
- Increased Blood Pressure
- Dizziness
- Tinnitus (ringing in your ears)
- Depression
- Erectile Dysfunction
So What is an NSAID and how much is too much?
NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) are a class of drugs, both prescription and over the counter, that decreases inflammation which then decreases pain. Not all OTC painkillers are NSAIDs. Acetaminophen, for example, is just a painkiller and does not suppress inflammation. Some studies have shown that toxicity can begin after one week of use at more than a half-gram a day. Keep in mind that the extra-strength pills are usually a half-gram EACH. Two pills three times a day is 3 grams – definitely not good for the ol’ liver.
How does an NSAID work?
This requires some talk about inflammation, which is best presented in a different blog. But I’ll boil it down here. In the body, inflammation is a major defense system against bugs and viruses. But it’s also the result of damage and is a part of the natural healing process. The mechanisms that cause and control inflammation are HUGE but there are two players worth knowing: COX-1 and COX-2. COX-1 is responsible for some housekeeping, protection, and regulation of various organs and processes. It’s a good guy to have around. COX-2 is responsible for the pain and swelling associated with inflammation. An NSAID works by stopping BOTH of them from working.
So when an NSAID prevents pain, it’s also preventing the protection and regulation of different areas in your body. How does this play out? In your stomach, COX-1 is responsible for making the lining that protects your cells. Poor stomach lining can lead to a bleeding ulcer which can remain completely painless and unnoticeable until one day you hemorrhage. Body-wide, the decreased inflammatory process leads to decreased immunity making your more susceptible to infections and sickness.
When is it okay to take an NSAID?
Like most things, everything is fine in moderation. For the occasional ache and pain due to a trip to the dentist or a rough day at work, an NSAID is great. But when you’re taking several handfuls for more than a week at a time, you’d be best served addressing the actual cause of the problem instead of just masking the pain that is caused by it.
Runner’s Knee
Hi everyone! Dr. Lell here. As Portland started getting warmer a few weeks ago, I saw the amount of people jogging by the clinic increase dramatically. Now I’m noticing more and more of something else – joggers with knee braces. This trend inspired today’s topic – Runner’s Knee.
This condition is closely related to Jumper’s knee and patellar tracking disorder and is one of the many conditions lumped in under the umbrella Patellofemoral Pain Syndrome/Disorder. That’s the thing about named conditions that I don’t like very much – the underlying mechanism of injury and pain is usually the same but the name will change depending on where in the body it is and what activity caused it. But I suppose people have to fill the pages of medical text books with something so there ya go. Before we begin, let’s cover the symptoms and relevant anatomy.
SYMPTOMS
In runner’s knee, there is usually pain at the top or sides of the kneecap after or during running, walking, jogging, jumping, climbing, or going up/down stairs. Sometimes there may be swelling and the discomfort can last a day or so.The pain may be located just below the kneecap on the shin; this is when we would call it jumper’s knee. Before we talk about what causes it, we should cover some basic anatomy so that you can really understand it.
ANATOMY
 The major players are:
The major players are:
- The patella (knee cap)
- The Tibia (shin)
- The Femur (leg bone)
- The Quadricep Tendon (attaches to the top of the patella)
- The Patellar Tendon (attaches to the bottom of the patella)
- The quadriceps (the muscles on the front of you leg)
That’s it. The external knee is pretty simple. There are two important things to appreciate and then you’ll completely understand this condition on a fundamental level. First, the patella is not actually secured into place like other joints (because it’s not a true joint). It’s just a bone that is being held in place with a good amount of tension by tendons on the top and bottom and it’s allowed to move a little bit in any direction whenever you bend your knee. Second, movement of this kneecap is caused by the quadriceps (a group of 4 muscles) that attach to the top and sides of the knee and limited by the patellar tendon at the bottom.
CAUSES
The fundamental cause of runner’s knee is muscle imbalance. The patella is a bone health in place mostly by tension wires. If the wires pull with an equal amount of tension in all directions, then the knee works fine. But if one wire pulls harder than the other, then the knee will be thrown off a little bit and this will, in turn, put tension on other areas and mess up the normal motion of the joint leading to abnormal wear and tear. It doesn’t help that there are some anatomical asymmetries of the knee joint and that some of those wires are a little pre-disposed to pull harder than others.
In some cases, the issue is coming from the ankle or hip. Think of the knee as part of a larger chain that transfers weight from your upper body into the ground and then absorbs the shock from that impact with each step. It’s hard to consider the knee without looking at the hip and ankle. But these joint or gait imbalances will set up a compensatory muscle imbalance around the knee joint. So the mechanics won’t change – just the underlying cause.
TREATMENT
Runner’s knee responds very well to conservative treatment like chiropractic care and physical therapy. When I treat someone with this condition, I try to first focus on the knee. Foam rolling the quads and general leg stretches (like this one) along with knee adjustments will do wonders to get the kneecap working properly again. If this doesn’t do the trick long term, it’s time to look above and below with hip stretches or maybe even an orthotic insert. It’s important to stretch before and after each run. If the knee is super-bad, then some simple rehab exercises may be useful balance out a muscle that may not just be tighter than the others, but stronger too.
If the knee is left untreated and activity levels don’t change, runner’s knee can create uneven and unnatural movement in the joint which causes degeneration and arthritis of the knee which can often become so severe that a total knee replacement may be needed.
Don’t let back pain ruin your sex life
Hello, all, Dr. Lell here. This blog is specifically geared towards women. If you’ve ever had low back pain, you know how hard it can be to live your normal life. Sometimes it works out to your advantage, “sorry I wish I could help you move this Saturday but my back is killing me.” Most of the time though it just keeps you on the couch and from doing what you want to do. By the way, waiting it out on the couch is the LAST thing I’d suggest for low back pain (LBP) but that’s another blog post. Even small things like shaving your legs and tying your shoes can seem like heroic feats. Clinically, you can always tell how bad the pain is and how long it’s been going on if a female patient arrives to the office with slip-ons and hairy ankles. LBP can seep in and affect almost every aspect of your life, even sex. Ever have back pain so bad that it hurt to drive in the car? Imagine how much worse a bumpier ride would have felt like. But like I tell my patients, “I’ll never tell you stop doing something you love, we just need to find a different way of doing it for the time being.”
Luckily in 2015, a couple of very smart people designed a small study to look at which sex positions caused the most motion in your low back. The authors, Sidorkewics and McGill published the work in the European Spine Journal. Positions studied were the quadruped position (all fours) with the weight being rested on both the hands and elbows, the missionary position with the hips are flexed up a little and a lot, and the side lying (spooning) position.
Looking at the lumbar spine’s motion during these activities are very important because several different conditions can cause LBP and each has their own characteristics. Some conditions and types of LBP hurt more when you bend over and others when you bend back. The different sex positions caused different motions in the lumbar spine.
So what’s the best sex position?
They found that the best position was the quadruped position (on all fours) with the weight resting on the hands (not the elbows). This caused the least amount of lumbar flexion which is exactly what you want to avoid in back pain caused by disc herniations (“slipped disc”) or discogenic pain just to name a few. This flexion intolerant back pain in the most common kind of back pain that we typically see in patients under 50 years of age. The worse position was missionary with the hips flexed up.
 Here’s the best safe for work image that I found. It was originally on womenshealthmag.com (one must give credit where credit is due)
Here’s the best safe for work image that I found. It was originally on womenshealthmag.com (one must give credit where credit is due)
Don’t let back pain stop you from living your life. Get out there and keep doing what you love.
I hope you’ve enjoyed this blog. Please post questions or comments if you have them and for more blogs about health and medicine, please subscribe!
You can see the abstract here:
http://www.ncbi.nlm.nih.gov/pubmed/?term=extension+intollerant+back
Shoulder Impingement
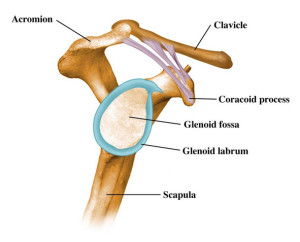
Hey everyone, Dr. Lell here. Today’s topic is shoulder impingement syndrome; a common condition that is often under investigated. There are four kinds of this condition but I’ll cover the most common one – Primary Mechanical Impingement. Let’s go over some of the simple anatomy first.
Basic Anatomy Of Shoulder Impingement
The important players are the
- The scapula (shoulder-blade),
- The supraspinatus muscle (posterior rotator cuff)
- A tunnel called the subacromial space. The space is what’s really important.
Take a look at the diagram. That unlabeled space above the fossa and below the acromion / clavicle is the subacromial space (let’s just call it the space).
That’s about as technical as we’ll get!
Causes of Impingement Syndrome
What causes impingement syndrome? -Anything that causes that area in the space to get smaller. The big three things that cause this are:
- The contents in the space gets bigger. There’s stuff in that tunnel. Most notably, the supraspinatus muscle and a bursa. If a person is using that arm a lot (swimming, working overhead, throwing), it can irritate and inflame that muscle. I usually see this in the younger athletic population.
- The walls of the tunnel get bigger. Years of wear and tear or a single large injury can change the joints and bones making the amount of free area in the space smaller. Alternatively, some people are born with a misshapen bone; this will have the same effect.
- The scapula isn’t stable during movement. The roof of the space is the scapula. The scapula isn’t strongly locked into place like other bones of its size. It’s held down by many muscles coming from many different directions. If those muscles are misbalanced, the scapula can have too much wiggle. This scapular instability or scapular dyskenesis is what I see the most of in non-athletic patients under 60; especially in people who sit at computers a lot.
Research Update!! Feb 27, 2020
Since this post, more information about shoulder impingement has come available.
Before, the common element of all scenarios causing impingement had to deal with the tendon getting aggravated or damaged by the bone on top. But someone looked at the tendons of people with various stages of impingement. They found that the first bit of damage occurs on the underside of the tendon, not the top (where the bony roof is). This suggests that a weakness or deconditioning of the tendon itself happens before the swelling and other factors.
What changes clinically?
With the new understanding, it’s very important to properly care for and recover from shoulder injuries. It’s also important to be able to move your shoulder fully without any discomfort or snags. These things will go a long way in preventing impingement syndrome. But if you already have it, care should focus on restoring pain free range of motion and exercises that strengthen the tendon. Easy band exercises go a long way in the clinic and home.
Welcome to the Blog!
Hello everyone. Dr. Lell here. I enjoy teaching and educating and am really looking forward to blogging as a means of reaching out to anyone with a question or interest.
You can expect blog topics to range from conditions, product reviews, and health tips to issues of public health. It’s my goal to explain all the ins and outs in an easy to understand way and usually with a few corny jokes. I’m always open to suggestions on topics or for answering questions so feel free to write in or drop a line on my facebook some time.